Unless you’ve been living under a rock, chances are COVID-19 has chewed your life up and even spit it out. Changing our way of life, to where we now face living in the ‘new-normal.’ But is COVID more of a concern for you with lupus?
Since late 2019, the pandemic has put fear in population groups throughout the world. No more so than in those deemed ‘high-risk,’ due to having such things as an autoimmune disorder.
It appears that those of us with systemic lupus face the same risk of COVID as the general population do. But, may have a tougher time. [1] Even though most lupus patients will be taking “hydroxychloroquine.” The now, notorious anti-malaria medication with possible preventive effects against COVID. [2]
The question is, do we have to wait for ‘herd immunity’ before we start living again?
No… in fact, here are three ways you can protect yourself against COVID.
What is COVID-19? – in the eyes of science
By now, many of us feel we have a good idea about COVID-19. But in case you have been living on a mountain top, let us have a quick lesson… through the eyes of science.
COVID-19 is part of the “Coronavirus” family. A large viral family that we’ve known to cause respiratory infections since the 1960s. [3] But may have existed well over 20,000 years ago. [4]
You may recall COVID’s cousins SARS and MERS causing havoc in 2003 and then 2012.
MERS, which is short for “Middle East Respiratory Syndrome” first came about in June 2012. Like COVID-19, it was first thought to have come from bats. Yet, we now know people contract it from camels. Hence, its more common name, “Camel Flu”. [5][6]
SARS takes credit for first bringing global fame to the coronavirus name.
Like COVID, “severe acute respiratory syndrome” began in China. But through people eating wild civet cats – rather than bats. Although the bats may have infected the Asian civet cats. [3]
SARS was the first coronavirus pandemic that spread from people-to-people by droplets. Of course, it isn’t the last. In fact, COVID-19’s official name is “SARS-CoV-2.” [3] Makes it seem like a lab project, doesn’t it?
How does COVID-19 spread?
As a rule, coronaviruses can maintain their infectivity for a few days in the environment. This does depend on different factors though. Such as environmental temperature, humidity, wind levels and exposure to ultraviolet radiation. [7]
Person-to-person
COVID can pass on from person-to-person via droplets from the mouth or nose of an infected individual. By speaking, coughing, sneezing, or singing for example. [8]
Contact with surfaces
Likewise, according to the World Health Organisation (WHO), transmission can also occur via surfaces. Let’s say, you happen to touch a surface or object that has virus particles on it. You can take on the virus by then touching your mouth, nose, or eyes. [9]
It is due to the lack of specific treatment, that WHO and governments around the world push preventive measures such as:
- Physical distancing
- Avoiding crowds of people
- Restraining from sharing personal objects
- Practicing “respiratory etiquette or hygiene” measures
- Washing hands with soap and water on a regular basis
- Applying alcohol gel
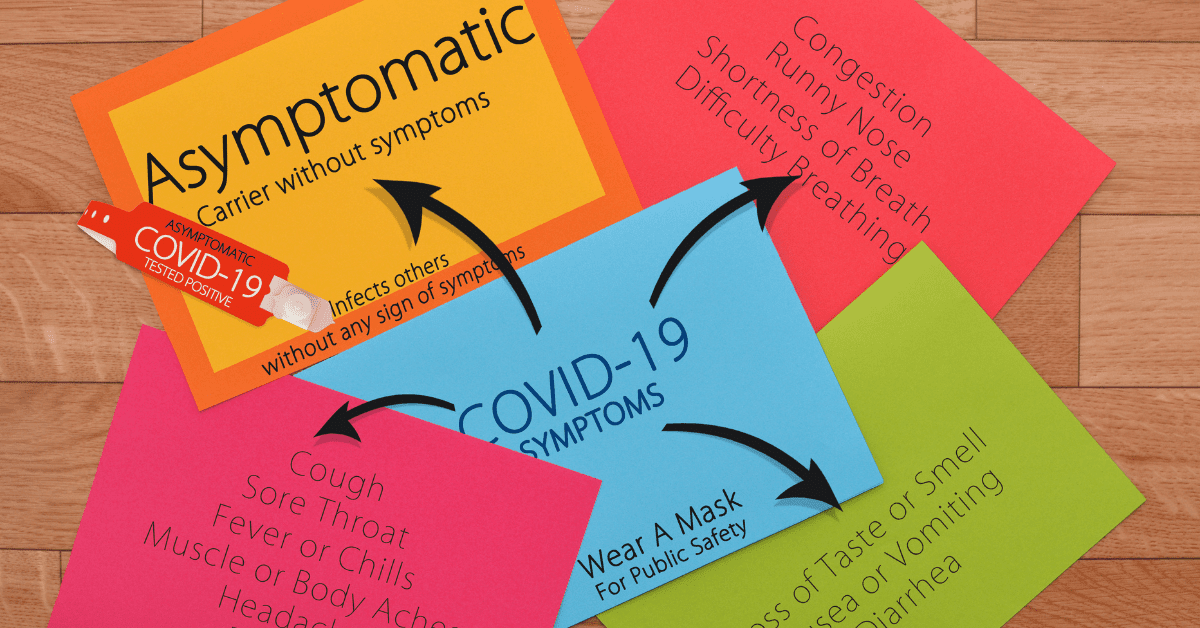
What are the Symptoms of COVID-19?
The WHO state that COVID affects different people in different ways. With most developing mild to moderate illness, which requires no medical treatment. [9]
Signs and symptoms of COVID-19 infection may appear after anything from 2–14 days. Yet, this does depend on the age and immune system of the affected individual. [10]
Most common symptoms:
- Fever
- Dry cough
- Tiredness
Less common symptoms:
- Aches and pains
- Sore throat
- Diarrhoea
- Conjunctivitis
- Headache
- Loss of taste or smell
- A rash on the skin, or discolouration of fingers or toes
Serious symptoms (need medical care):
- Difficulty breathing or shortness of breath
- Chest pain or pressure
- Loss of speech or movement
Still, those with mild COVID could still have it up to eight days after symptoms disappear. [11]
With fatigue lasting up to 10-weeks in some cases. [12]
Why does Science suggest COVID-19 is Dangerous?
All the hysteria about COVID-19 is understandable when you consider its close relatives.
SARS was contagious and spreadable via droplets – clocking over 8,000 cases in China alone. Whereas MERS wasn’t as contagious but had a high death rate of 32.97%. [8] Making for scary news if COVID-19 was to be the worst of both viruses – or worse.
But as we learn more. It begs the question, “Is COVID-19 dangerous enough to shut the world down?” Or even forcing people to vaccinate?
High Death Rate
In 2020, 1.83 million died from COVID-19. With an extra 980,000 joining the list from the first three months of 2021. [9]
In England and Wales, COVID-19 was on the death certificate of 80,803 deceased individuals in 2020. That’s an average of 221 people a day. With the figure going up to 134,597 by mid-March, 2021. [9]
Worrying figures by anyone’s standards.
But…
You should take this data with a pinch of salt. As COVID deaths may be lower.
For instance, ONS keep track of how many death certificates have COVID-19 on them. But they do not define whether COVID was an underlying cause of death or not.
An independent study shows COVID did not play a role in around one out of every 13 “COVID-related deaths.” Being as high as one third in some cases. [13]
Then we have different definitions and criteria throughout the world. So, one country may only record COVID hospitalisations. Whereas another nation will count all positive tests. Yet, the statistics will go against one another on the global stage. [14]
Still, if you wish to see the figures now you can use the UK government dashboard or WHO’s COVID data map.
Worse than the flu – (for now)
One comparison that pops up a lot is COVID-19 and the influenza virus… AKA the flu.
Mathematical models predict that within 10-years, COVID-19 could become little more than a nuisance. Causing no more than common cold-like coughs and sniffles. But not due to how the virus will mutate, but how our immune systems will adapt. [15]
Until then, COVID-19 appears to be a threat to our health and wellbeing. More so than the flu. One study suggesting COVID-19 has a higher rate of complications and mortality. These include: [16]
- Respiratory insufficiency
- Pneumonia
- Acute kidney injury
- Acute heart failure
Influenza and COVID-19 do have their similarities though.
For instance, both viruses spread via contact, droplets and contaminated surfaces. [17] They can both also cause respiratory disease. From mild sickness to severe cases that result in death. [18] COVID-19, like the flu, could cause heart inflammation. [19][20] But, this is yet to be certain, and may even be a result of the vaccine. [21][22]
Long COVID
It does appear that for now at least, the long-term effects are worse for COVID-19.
For example, the flu can last up to 9 days in children – the highest affected. [23] Yet, COVID-19 health issues could drag out beyond six to eight months. [24]
This is what we refer to as, “long COVID.”
Long-term Issues include: [25]
- Fatigue
- Breathlessness
- Psychological distress — including problems with concentration and memory
- A general decline in quality of life
- Higher risk of death [26]
New Mutations
You can’t go a week without the news of a new ‘variant’ sweeping the world. The ‘Delta variant’ being the sponsored version as I write.
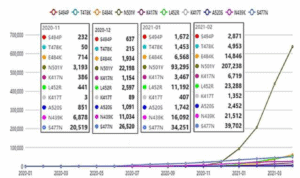
Scientists know all viruses mutate to survive. Why else develop the COVID-19 virus mutation tracker? [27]
The “SARS-CoV-2” virus makes around one or two mutations a month. This sounds quite a low number and is in fact lower than for other viruses – including influenza. [28]
The more the virus circulates, the more opportunity it has to change. [29] This, in theory, supports the effort to suppress the spread of the virus by any means necessary. Hence, social distancing, mask-wearing and handwashing etc.
Can vaccines create versions?
Mutation rates evolve in response to specific selective pressures. [29]
Vaccines could be one possible ‘pressure’ as they can drive viral mutations. Meaning COVID-19 vaccines may add fuel to the mutations of coronavirus. Rather than kerb it. As suggested by Professor Paul Bieniasz from Rockefeller University, USA. [30]
This could explain why there was a surge in the number of mutated variants from December 2020. The time mass vaccination programmes began. The 11 months running up to November 2020 were slow in comparison (see below). [31]
This could explain why current vaccines are vulnerable to new variants. Highlighting a need for mutation-resistant vaccines. [32]
Remember, Only the Strong Survive
With that said, certain mutations will make the virus stronger – thus harder to defeat. Whilst, some mutations weaken the virus – helping us to handle the virus with ease.
For example, one research found the virus mutated to make it 10-times more contagious. But as a result, more susceptible to a vaccine. [33]
But other studies show the virus can evade the immune system thanks to certain mutations. [34][35] One of which is a result of the virus deleting small bits of its own genetic sequence. [36] Avoiding your body’s natural anti-viral arsenal that it deploys in such instances.
In all, the current ‘Delta variant’ carries eight different mutations. Which together increase its ‘viral fitness’. Meaning it can infect lung and intestinal cells with less effort. Supporting the need to research new vaccines or booster vaccines. [37]
Could COVID Trigger an Autoimmune Disorder?
In critical cases of COVID, patients can develop septic shock and/or organ damage.
This includes: [38]
- Skin
- Kidneys
- Respiratory System (breathing)
- Cardiovascular System (heart)
- Digestive system (stomach)
- Nervous system
- Haematological system (blood and bone marrow)
Cytokine Storm
The immune system response is similar in autoimmune diseases and critical COVID-19. With organ damage in both diseases being immune-mediated. [38]
One such immune response is to send out immune cells called “cytokines.” These alarm signals put your body into ‘inflammation mode.’
Similar to a spy, their job is to hunt for a virus to call in the artillery.
Have too many floating around in your blood, and you have a “cytokine storm” on your hands. Named as such, because when this happens the immune system rips through the body like a tornado. Causing all sorts of damage – and even death. [39]
B-cells
Research papers on COVID-19 also highlight that “autoantibodies” may play a role.
Rogue antibodies can attack your body’s immune defences, tissues or organs. Resulting in targeted, longer-term damage. That is, in comparison to the short-mayhem that cytokine storms can cause. [40][41][42]
A source of antibodies in your body are the white blood cells known as, “B-cells.” The ‘B’ stands for bone marrow, where they begin their life.
B-cells become ‘activated’ when they come across a foreign invader. Acting like a radar beacon to tag enemies for the immune system to attack.
Sometimes, B-cells become rogue and produce antibodies against your own cells. Bypassing the checks and balances that are in place to constrain them. This is what researchers have seen happen with COVID-19.
COVID also resembles what takes place in autoimmune conditions like systemic lupus. [43]
In fact, a 39-year-old man had clinical signs of lupus 2 months after getting COVID-19. [44]
But this shouldn’t come as too much of a shock as viral infections are one suspected trigger of lupus. People may develop lupus after an acute Dengue Fever Virus infection, for instance. [45]
Something to note as I went to Cape Verde less than a year before my diagnosis of systemic lupus.
– CLICK HERE to learn what can cause Lupus –
What is your risk of getting COVID with Lupus?
The general advice is that immune suppressors put you at a higher risk of viral infections. As they weaken the immune system, which makes sense.
Yet, whether having lupus increases your risk of catching COVID-19 is still up in arms.
Some scientists suggest that if you have lupus, you’re high-risk. [46] Whilst others say otherwise. [1] Regardless of whether you’re taking immune-suppressing medications or not. [47]
If anything, steroid medications appear to be more of a factor in how it affects you. [47][48]
As could, the now notorious, “hydroxychloroquine.” That many of us with lupus take on a regular basis. A favourite of the then, President of the United States, Donald Trump. Which we know has the potential to combat COVID. [2]
So, we face a similar threat to what the general public does.
In fact, scientists now suggest that severity may come down to your nose and throat.
With a blunted nasal response being to blame. Allowing the virus to enter the body uncontended. [49]
How can we combat COVID?
The good news is that most of us will face mild-to-moderate COVID symptoms.
Plus, even though COVID-19 is a new disease, the immune system can fight back. Like how the body responds to the flu. [50]
One study claims that mild-COVID leaves a long-lasting protective effect. Showing that antibodies were still present in people 11-months after contracting COVID. [51]
But as always, prevention is better than cure.
So, if you can, avoid COVID.
But you can at least prepare your body for battle by taking the following steps:
1. Antioxidants
To know the benefit of antioxidants, we need to understand how COVID-19 infects cells.
How COVID-19 Infects Cells
Picture a sea mine – like the one in the 2007 film, Hot Fuzz. This is what the COVID-19 virus looks like under a microscope.
Surrounding the virus are protein spikes that attach to certain receptors called “ACE2”. These receptors live on the surface of cells within your respiratory tract… which starts with your mouth and nose and ends deep in your lungs. This process allows the virus to enter the cell and start making new copies of itself. The copies then go on to infect other healthy cells.
One main anchor for these protein spikes may be the “disulphide bond.” This is a unique bond that forms between two ‘cysteine’ amino acids.
This special bond only occurs in animals susceptible to the COVID-19 virus. For example, humans, cats, and dogs. But does not form in animals resistant to the virus, like pigs and cows. [52]
An ‘oxidizing cellular environment’ keeps this special bond together. And it is possible that this occurs more in the elderly or those with health conditions. Giving them the ideal environment for COVID-19 to infect and spread.
Preventing this anchor from forming could be a key tactic in battling COVID-19. Done so by disrupting the ‘oxidising environment’ that keeps the disulphide bonds intact. This is where antioxidants could come in.
What to do:
You can buy antioxidant supplements from most health shops.
But a supplement may contain one type of antioxidant or even several. Yet, your food can contain thousands of types of antioxidants.
So avoid supplements and choose food.
Some good natural sources of antioxidants are:
- Berries: Blueberries, blackberries, raspberries, strawberries and cranberries
- Beans: Small red beans and kidney, pinto and black beans
- Fruits: Many apple varieties (with peels), avocados, cherries, green and red pears, fresh or dried plums, pineapple, oranges, and kiwi
- Vegetables: Artichokes, spinach, red cabbage, red and white potatoes (with peels), sweet potatoes and broccoli
- Beverages: Green tea, coffee, red wine and many fruit juices
- Nuts: Walnuts, pistachios, pecans, hazelnuts and almonds
- Herbs: Ground cloves, cinnamon or ginger, dried oregano leaf and turmeric powder
- Grains: Oat-based products
- Dessert: Dark chocolate (high cacao content)
– Antioxidants are a complex subject – so CLICK HERE to learn more –
2. Good Gut Health
Being obese is a risk factor for severe COVID.
The reason why could be due to fat having high numbers of ACE2 receptors (as mentioned above). Making fat tissue a prime reservoir for COVID-19.
Leaky Gut AKA “Increased Intestinal Permeability”
“Leaky gut” plays a big role in obesity – as it does with diabetes and insulin resistance.
This is when your internal piping develops cracks. Allowing its contents to spill into your circulation.
This includes intestinal bacteria and their toxins. Both of which appear at high levels in the lungs of obese people – even without an infection.
So, could COVID be the straw that broke the camel’s back?
Adding enough damage to create a more severe infection. [53]
A leaky gut will allow the virus to reach the outside of your digestive tract – and internal organs.
Organs are vulnerable to infection because they are also rife with “ACE2” receptors. [54] Raising your risk of severe COVID-19 even more.
Bad Bacteria
An unhealthy gut could be another reason why some people have such severe infections. Well, according to a review by a Korean researcher at least. [54]
Poor gut health has links to two COVID risk factors: old age and chronic conditions. Most likely due to the ‘western diet’ of low fibre, high fast food.
Also, COVID-19 infection appears to happen more in guts low on certain bacteria families. Ones that produce “butyrate”… a ‘short-chain fatty acid’ that plays an important role in gut health. More so by reinforcing the “gut-barrier function”. [54]
Lupus’s link to Long COVID
The gut is the largest immunological organ in the body. Its resident microbes can influence your immune responses. Meaning that your gut make-up will play a role in how you respond to COVID.
One study saw lower levels of certain species in those with COVID. Ones that can influence your immune system response. Such as Bifidobacterium adolescentis, Faecalibacterium prausnitzii and Eubacterium rectale.
With less “F. prausnitzii” and “Bifidobacterium bifidum” influencing infection severity the most. A possible decisive factor behind Long COVID. [55]
An interesting find from this study was the higher numbers of “Ruminococcus gnavus.” [55] A family of bacteria that appears to be five times higher in women with lupus. [56] As well as lupus-prone mice. [57]
What’s more, R. Gnavus can feed off “mucin”. A key building block for the protective mucus lining of our guts. [58] Making it a potential cause of “leaky gut”.
What to do:
- Eat more dietary fibre if you consider yourself to eat very little fruit and vegetables. Especially the dark green leafy type.
- Take probiotics focusing on butyrate-producing gut microbes
- Consume ‘butyric acid’ rich foods like ghee, raw milk, kombucha, and/or Jerusalem artichokes. Or take it in supplement form.
– Click Here to Learn More on how dietary fibre can improve lupus –
3. Vitamin D
Taking 400 to 1000IU a day of Vitamin D can protect you against acute respiratory infections. Suggesting that Vitamin D may guard you against COVID-19. [59][60] Although, some do dispute this. [61]
In one study, 80% of COVID-19 patients had a Vitamin D deficiency. [62]
What’s more, this study was in Spain, where you would think Vitamin D deficiency wouldn’t be an issue. This is because Vitamin D develops in the human skin due to sunlight exposure. Yet, it appears it is – especially in the older age group. [62]
In fact, sunny countries like Spain and Northern Italy seem to have low Vitamin D. Alongside greater rates of Vitamin D deficiency. Whereas Nordic nations such as Norway, Finland and Sweden have higher Vitamin D levels… even though they have less sun. A result of supplementation and the fortification of foods.
This could explain why Spain and Italy had higher rates of COVID-19 infection and death rates. Suggesting that Vitamin D could boost your immunity against COVID-19, and other infections. [63]
Vitamin D is close to being risk-free
In truth, we need better studies before this can be conclusive.
But to be honest, the population, in general, should take a daily supplement containing 800–1000 UI. It has benefits and should not do any harm. [64]
Still, some medicines can interact with Vitamin D. So, speak to your doctor if you are taking these tablets. [65] More so if you’re on statins, anti-tuberculars, and anti-epileptics.
Also, Vitamin D toxicity, although rare, is possible. It can cause dehydration and result in high calcium levels – at an expense of your bones.
But an important tip. Take magnesium with your Vitamin D supplement. This is because magnesium is essential in the metabolism of Vitamin D. [66]
What to take:
800-1000IU a day of Vitamin D should do – alongside a Magnesium supplement.
Pingback: What Causes Lupus? (An up-to-date answer in 2021) -